TMS Therapy for Depression
Transcranial Magnetic Stimulation or 'TMS' is a fast-acting and sustainable treatment for Depression and OCD. neurocare utilizes a personalized approach, with TMS accompanied by a focus on psychotherapy and sleep hygiene, which has been proven to demonstrate enhanced response and improved remission rates.
.png?width=1480&height=500&name=tms-therapy-rebates-in-australia_hd%20(1).png)
Between 30-50% of people with depression either do not respond to antidepressant medications or make the decision to discontinue it due to side effects. At neurocare we offer a medication-free alternative for treating mood disorders like depression and OCD, known as Transcranial Magnetic Stimulation (TMS).
TMS is a fast-acting and sustainable treatment that works by delivering magnetic pulses to alter the activity within the brain networks that regulate mood.
This process allows us to influence activity in your brain and not only relieve your symptoms but to address the problem at its core.
TMS at neurocare is psychologist-lead with accompanying psychotherapy support in session.
TMS is endorsed by the Royal Australia & New Zealand College of Psychiatrists for the treatment of depression and OCD.
How does TMS work?
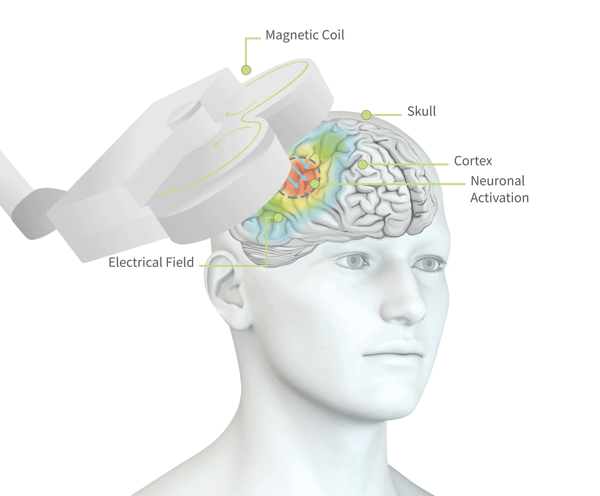
Treatment involves positioning a magnetic coil on your head which delivers a pulse to stimulate specific regions of the brain. The magnetic pulse stimulates nerve cells in a region of your brain involved in mood control and depression.
TMS works particularly well and is highly recommended for those who have not responded to traditional medication for depression or OCD. This type of treatment also avoids the side effects associated with antidepressant medications.
Who can benefit from TMS?
TMS in Depression
TMS is a reliable and efficient treatment for depression. It is highly recommended for individuals who have not seen improvement with medication or other treatment methods.
TMS is also a treatment option for patients seeking to reduce their dosage of antidepressant medication or by those aiming to discontinue medication completely. This course of action should be closely monitored and supervised by a medical professional.
TMS at neurocare is psychologist-lead with in-session psychotherapy for more effective outcomes and improved remission.

TMS in OCD
TMS is also a potential solution for individuals struggling with Obsessive-Compulsive Disorder. Similar to its use for patients with depression, this treatment is especially beneficial for patients who have not found success with other therapies.
Studies conducted by neurocare clinics in the Netherlands found that the response rate of TMS therapy for patients with OCD was 55%. A personalized approach to TMS, whereby the patient was also closely monitored to improve their sleep hygiene, is also understood to improve response to treatment.
This technique of combining TMS with psychotherapy and other forms of assessment can be particularly effective.
To find out more about TMS and the research behind it, visit our Scientific Publications page.
Advantages of TMS
Medicare rebates available
TMS therapy is listed on the MBS for treatment of depression that has not responded to antidepressant medications or psychotherapy. This means better outcomes and a better quality of life for more people.
Medication free
Two-thirds of people with depression don’t get adequate relief from the first antidepressant they try, and each subsequent medication tried is less likely to help than the one prior. For those looking for a medication-free treatment for depression, TMS is a highly effective option.
Safe, with minimal side effects
The stimulation used in TMS is safe and well-tolerated. Treatment has no negative effects on thinking, memory, or any other normal brain functions. Unlike other treatments for depression, TMS does not cause weight gain, sexual dysfunction, nausea, cognitive dulling, or withdrawal effects.
Fast and long-lasting
An average of 20 sessions is typically needed, with sessions held at least twice per week. Positive effects may be noticed within the first 10 sessions, and after a full course of TMS treatment many individuals enjoy long-lasting relief from symptoms.
Convenient outpatient treatment
TMS is a focused stimulation technique (unlike therapies like ECT), with no need for sedation or anaesthesia. Individuals are awake and alert the entire time, and immediately able to resume their everyday activities at the end of each treatment session.
Supported by science
We only apply protocols that have shown clinical efficacy. By combining TMS with psychotherapy, 66% of clients in our global clinic network, who suffered treatment resistant depression, responded to treatment and significantly decreased their symptoms.
What to expect when doing TMS therapy

For best results, TMS sessions need to be scheduled daily or at least three times a week. Some patients report antidepressant effects after 5 sessions, however, it’s important to remember that, just as individual causes of depression differ, so does the response to treatment. neurocare recommends between 20 to 30 sessions to consolidate the antidepressant effects. You can complete a full course of treatment within one to two months.
At neurocare, TMS sessions are either delivered as 45- or 30-minute appointments. In all sessions, psychotherapy with a psychologist is included.
The sessions are conducted in a comfortable treatment chair, where a magnetic coil is placed over your head. The coil generates a pulsating magnetic field, stimulating the target areas within the brain. The magnetic field generates a noticeable ticking sound. While the stimulation is not painful, many patients notice a tingling sensation on their scalp.
Frequently Asked Questions about TMS
-
Independant scientific efficacy
TMS is endorsed by the RANZCP as an effective treatment for major depressive disorders and multiple scientific reviews have found consistent evidence that TMS provides a clinically relevant benefit to patients with treatment-resistant depression.
neurocare follows an evidence-based approach to treatment which combines TMS with psychotherapy. This combined approach maximises the brain’s natural ability to change and recover and has been shown to deliver positive results and significantly decreased symptoms in 66% of patients.
After six months, a remarkable 65% of patients in this research still reported long-lasting remission from depression.
Results from neurocare's global research team
Our research studies show that after approximately 20 sessions, two-thirds of clients experience a significant improvement in their mood symptoms. The best results are based on a combined treatment using both rTMS and psychotherapy.
-
TMS is not the same as electroconvulsive therapy (ECT).
In ECT large electric currents are applied to create seizure activity across the brain. This therapy requires sedation under medical care in a hospital, and may be associated with side effects including nausea, confusion, and memory loss.
TMS stimulation is very light and focused, so it doesn’t affect the whole brain or create a seizure. After a TMS session you can safe return immediately to your daily activities including driving, studying, and work.
-
On average our clients need about 20 TMS treatment sessions. For the best results treatment sessions should be held at least 3 times a week. You may start to notice an effect within the first 5 sessions.
-
TMS has the advantage of not inducing side effects common with anti-depressant medications.
Treatment is not painful. Those undergoing TMS describe the magnetic pulses as a tapping, tingling, or twitching sensation.
-
TMS in combination with psychotherapy has been found to last at least six months for the majority of clients.
A number of clients will opt to return for follow-up treatment once a month or once every 2 to 3 months to maintain the effects or to prevent relapse.
Research shows that after six months depressive symptoms are significantly lower than at intake.
-
You do not need a referral to start your treatment as a private client, however you will not be able to claim treatment from Medicare without a referral.
If you would like to claim either your TMS sessions or any Psychology or Psychiatry sessions, you will need a referral from your GP. Our friendly intake team can let you know what type of referral you might need.
-
Up to 30 sessions of TMS are eligible for a Medicare rebate for people diagnosed with treatment-resistant major depression.
Note: There are certain criteria required to be eligible for Medicare funding for TMS. To find out more, please speak to our friendly intake team.
-
It is generally recommended to keep medications stable during the course of a rTMS treatment program, and to inform the clinical staff of any changes in medication use.
Always talk to your prescribing doctor about changing medication. You are still able to do TMS sessions while taking or reducing medication.
-
A QEEG brain mapping session may be recommended for two reasons. The first is safety. Our clinicians review the QEEG results to rule out any patterns of brain activity that could suggest an increased risk of seizure.
A QEEG assessment also allows us to further personalise your treatment, by identifying additional factors which may be contributing to depressive symptoms (e.g. a sleep disorder).
-
Unlike some medications, TMS does not affect your ability to drive. The experience of intensive treatment, however, can be tiring. If you would not feel comfortable driving after this experience, we advise you to ask a friend to drive you home after a treatment session.
Not sure if our services are right for you?